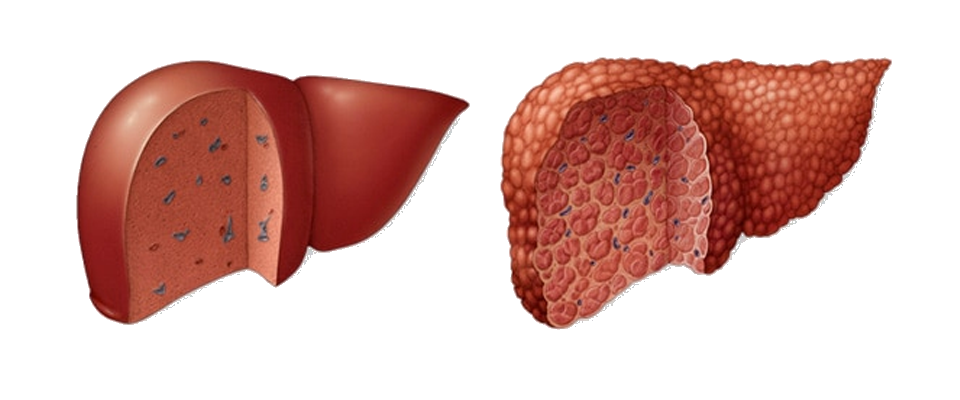
I have been aware that I have had a fatty liver for some time…. Although my liver function is fine, ultrasounds over the last few years have shown that it is enlarged (which is not unusual with obesity) and a Fibroscan undertaken last year indicated that it was probably scarred (and potentially cirrhotic), but it was not until a liver biopsy was taken during my gastric bypass surgery, that Cirrhosis of the liver has been confirmed.
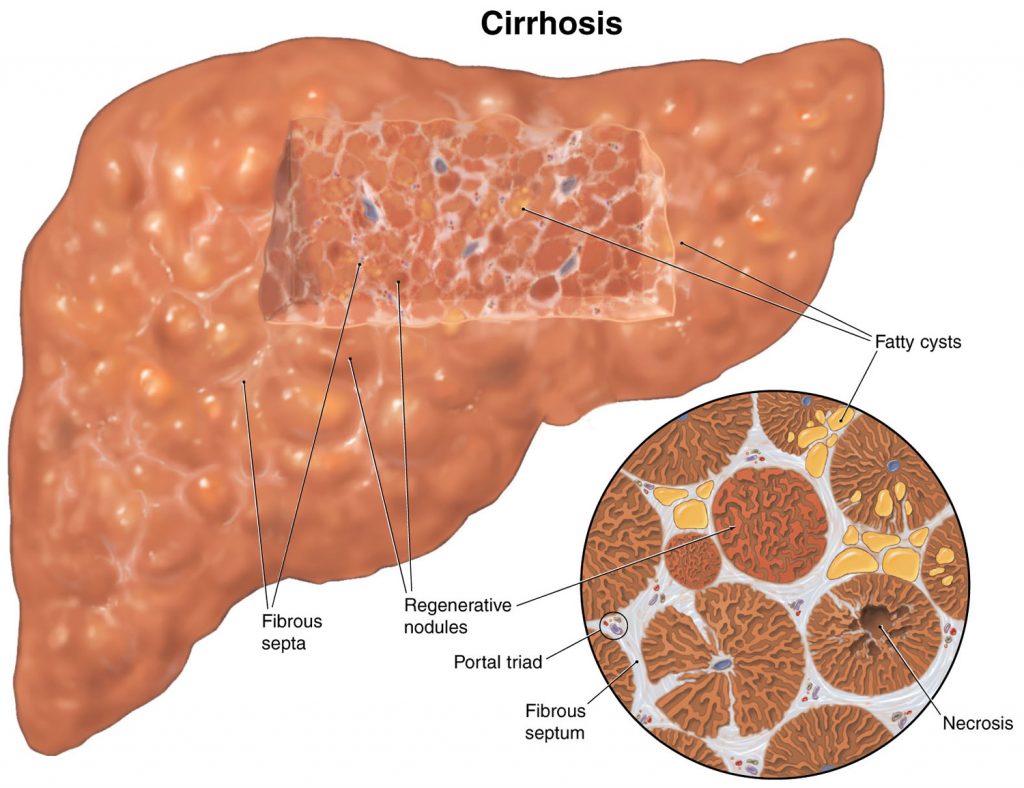
Cirrhosis is scarring of the liver caused by long-term liver damage. … Cirrhosis can eventually lead to liver failure, where your liver stops working, which can be fatal. But it usually takes years for the condition to reach this stage and treatment can help slow its progression.
Cirrhosis is a type of liver damage where healthy cells are replaced by scar tissue. The liver is unable to perform its vital functions of metabolism, production of proteins, including blood clotting factors, and filtering of drugs and toxins. A common misconception is that liver cirrhosis is caused by drinking excessive amounts of alcohol, but there are a number of other ways that the liver can be damaged and lead to cirrhosis.
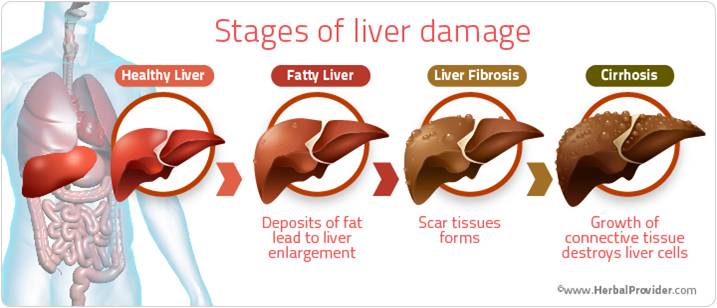
Liver cirrhosis and fatty liver
Non-alcoholic fatty liver disease (NAFLD) is a condition where fat accumulates in the liver. It now affects about 20 per cent of Australians. It is becoming more common in children who are overweight or obese. Fatty liver does not usually cause pain or nausea. NAFLD is associated with conditions such as:
- obesity – 20 per cent of people with obesity have fatty liver disease
- high blood cholesterol and triglycerides
- type 2 diabetes.
NAFLD can lead to inflammation of the liver and the formation of scar tissue, a condition called non-alcoholic steatohepatitis (NASH), which can then lead to cirrhosis of the liver. NASH usually occurs in people who are obese, have diabetes or have high blood cholesterol and triglycerides, so controlling these conditions is recommended.
Complications of liver cirrhosis
Without medical treatment, cirrhosis of the liver can lead to a range of potentially life-threatening complications including:
 insulin resistance and type 2 diabetes – a poorly functioning liver stops the body from properly using insulin, the hormone that moves sugar from the blood into the cells
insulin resistance and type 2 diabetes – a poorly functioning liver stops the body from properly using insulin, the hormone that moves sugar from the blood into the cells- osteoporosis (brittle bones) caused by changes to metabolism of calcium and vitamin D
- primary liver cancer – the most common type of cancer caused by cirrhosis is hepatocellular carcinoma
- liver failure – scar tissue can impair the functioning of normal liver tissuebleeding from blood vessels in the oesophagus or upper stomach (oesophageal varices)
- increased blood pressure in veins that take blood to the liver (portal hypertension)
- build-up of fluid within the abdominal cavity (ascites)
- infection of the fluid found within the abdominal cavity (spontaneous bacterial peritonitis)
- damage to the brain and nervous system caused by toxins that the liver has failed to remove (hepatic encephalopathy).
Treatment of liver cirrhosis
Cirrhosis of the liver is incurable but, in some cases, treatment can help to reduce the likelihood that the condition will become worse. Options include:
- treating the underlying cause of liver damage
- making dietary and lifestyle changes – a nutritious low-fat diet, high-protein diet and exercise can help people to avoid malnutrition
- avoiding alcohol – alcohol damages the liver and harms remaining healthy tissue
- Taking certain medication – such as beta-blockers to reduce blood pressure and lower the risk of bleeding, diuretics to remove excess fluid
- avoiding certain medication that can make the symptoms worse – such as non-steroidal anti-inflammatory drugs (NSAIDs), opiates or sedatives
- having regular medical check-ups – including scans to check for liver cancer
- having regular endoscopic procedures to check whether there are varicose veins within the oesophagus or stomach
- having a liver transplant – an option that may be considered in severe cases.