by Me | Dec 4, 2019 | Diabetes, Exercise, Fatty Liver
Despite being the fittest, healthiest and skinniest I have been for more than 30 years… and in fact, quite probably because of it, I have been dumped multiple times in the last few months !!!
I have had several people, who have played an important part in my life over the last few years, who have decided that our relationship is no longer necessary and that they no longer want to see me on a regular basis !!!
But it is not actually a bad thing… in fact it is a very good thing.. because it is my medical specialists who are “dumping” me in droves…. They have determined that because my health has improved so dramatically over the last 12 months, that there is no longer any reason to see me on a regular basis… and that just an occasional catch up (if that) will do fine.
Endocrinologist
As I have been completely Diabetes medication free for over 12 months (since the day after surgery), and my Blood sugar is well within the “normal” range, my Endocrinologist has declared me “Diabetes Free” and told me not to come back…
Liver Specialist
My Liver specialist says that despite permanent scarring (from Cirrhosis), my Liver is functioning beautifully and my blood data is giving no indication of liver problems at all. She suggests that I touch base in 6 months or so.
Bariatric Surgeon
My Surgeon and Dietician are VERY happy with the outcome of my surgery (62 weeks ago) – and so am I… I weigh nearly 10Kg less than I once thought possible and am still losing weight…. I will catch up with them in another 6 months or so too.
General Practioner
Even my GP is not in any hurry to see me again 🙂
My Gym Trainer/s
The only relationship which I am still fostering is with my trainers at the gym…:) … but even that might be on a downward trend, as I have determined that my Passion for Excercise (NOT an Obsession – I promise) maybe just a little excessive and am considering reducing my 6 or 7 workouts a week (although I am tempted to start swimming as well).
Perhaps I should consider establishing a NEW relationship…. with a Plastic Surgeon…. for an Abdominoplasty – Joking !!! (at the moment) ….
by Me | Oct 22, 2018 | Fatty Liver
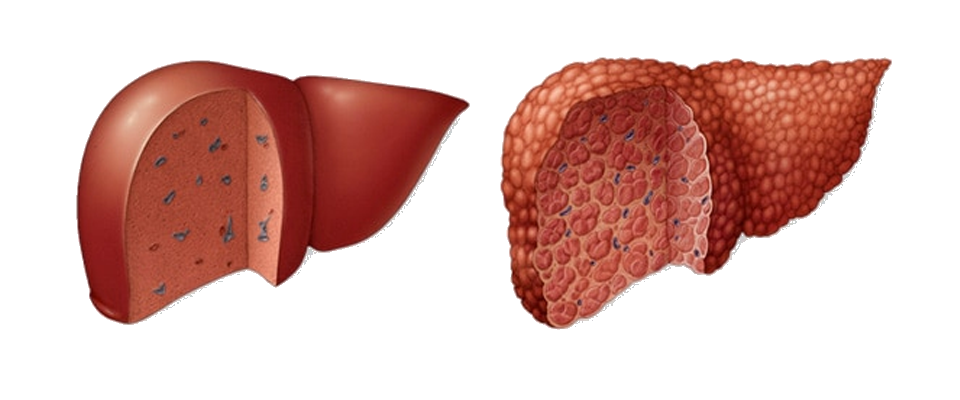
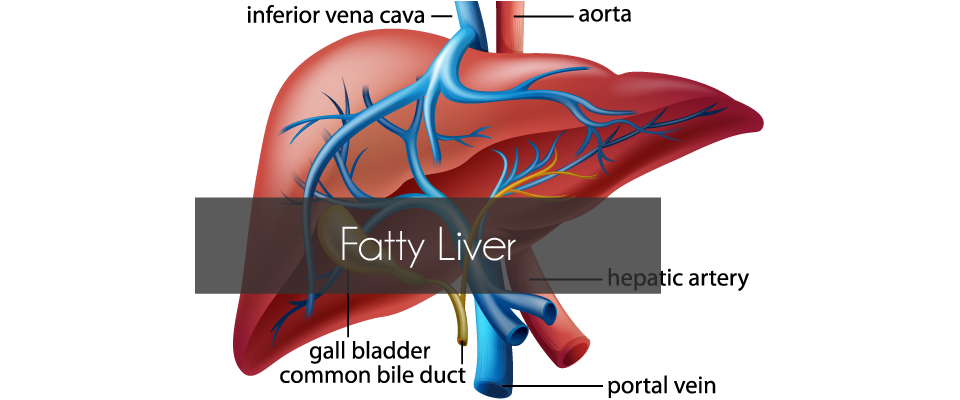
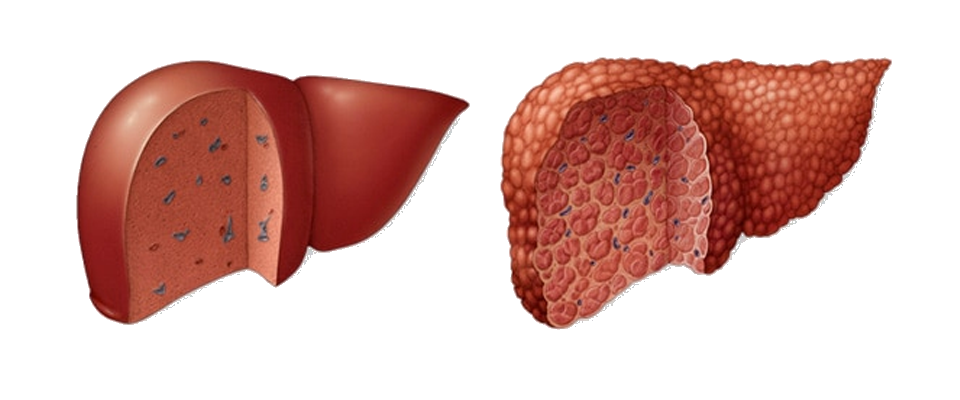
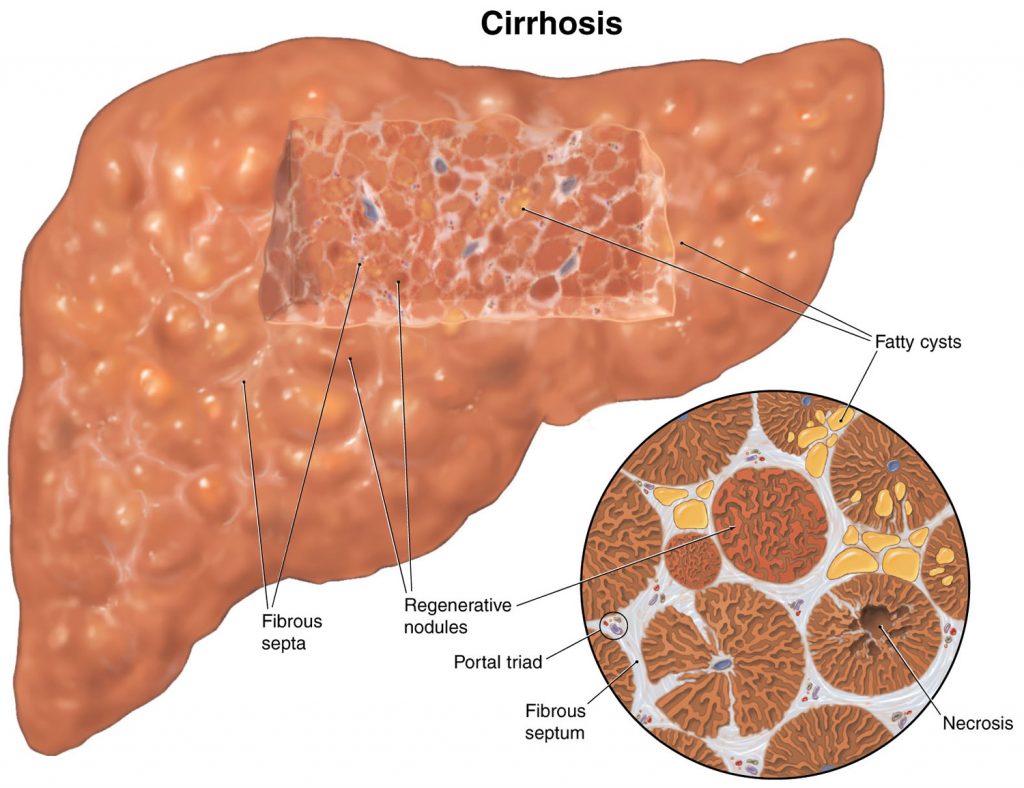
I have been aware that I have had a fatty liver for some time…. Although my liver function is fine, ultrasounds over the last few years have shown that it is enlarged (which is not unusual with obesity) and a Fibroscan undertaken last year indicated that it was probably scarred (and potentially cirrhotic), but it was not until a liver biopsy was taken during my gastric bypass surgery, that Cirrhosis of the liver has been confirmed.
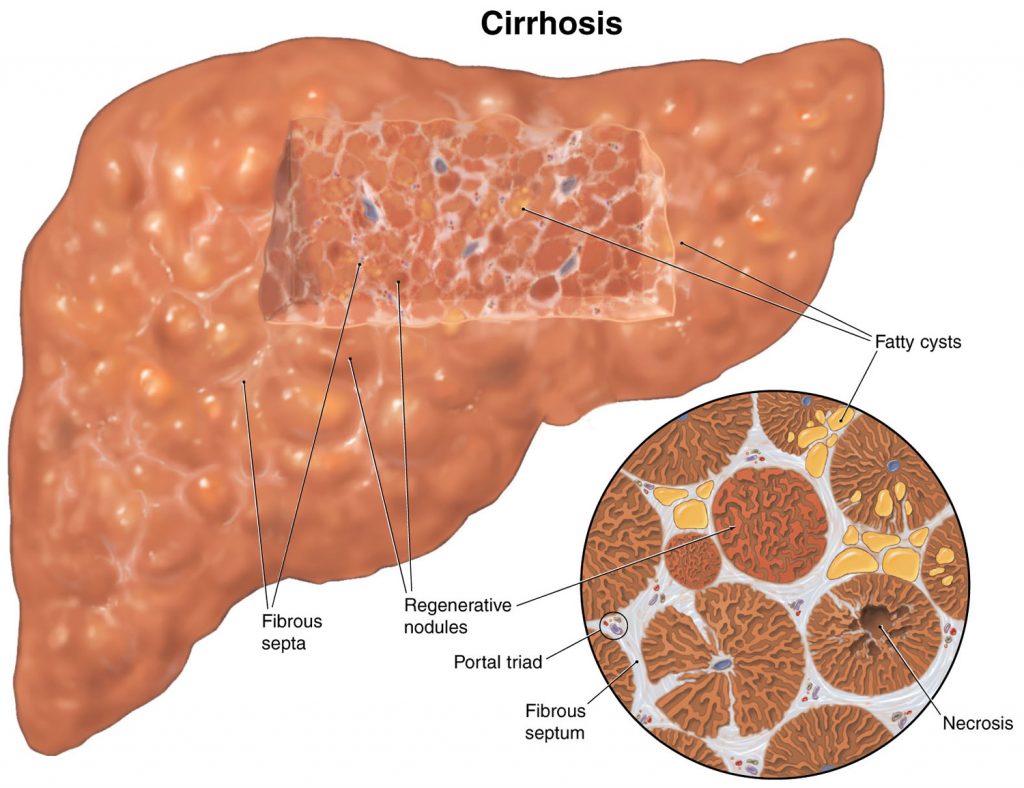
Cirrhosis is scarring of the liver caused by long-term liver damage. … Cirrhosis can eventually lead to liver failure, where your liver stops working, which can be fatal. But it usually takes years for the condition to reach this stage and treatment can help slow its progression.
Cirrhosis is a type of liver damage where healthy cells are replaced by scar tissue. The liver is unable to perform its vital functions of metabolism, production of proteins, including blood clotting factors, and filtering of drugs and toxins. A common misconception is that liver cirrhosis is caused by drinking excessive amounts of alcohol, but there are a number of other ways that the liver can be damaged and lead to cirrhosis.
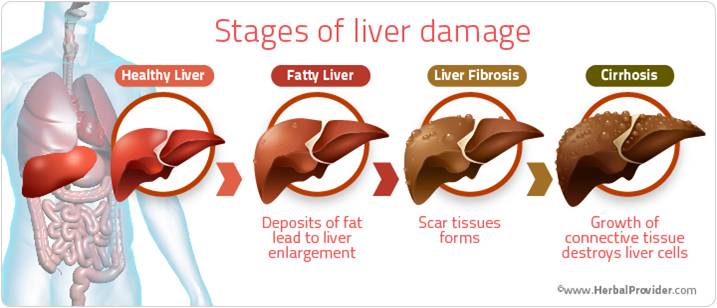
Liver cirrhosis and fatty liver
Non-alcoholic fatty liver disease (NAFLD) is a condition where fat accumulates in the liver. It now affects about 20 per cent of Australians. It is becoming more common in children who are overweight or obese. Fatty liver does not usually cause pain or nausea. NAFLD is associated with conditions such as:
- obesity – 20 per cent of people with obesity have fatty liver disease
- high blood cholesterol and triglycerides
- type 2 diabetes.
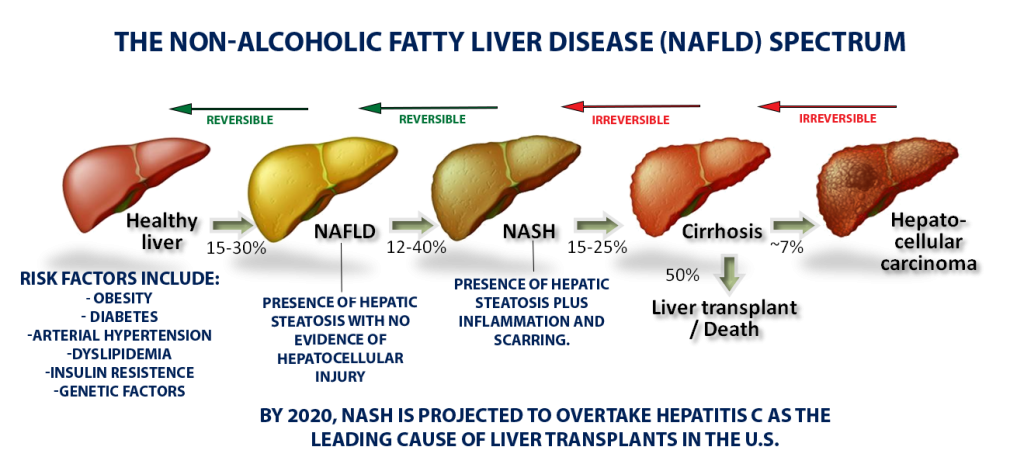
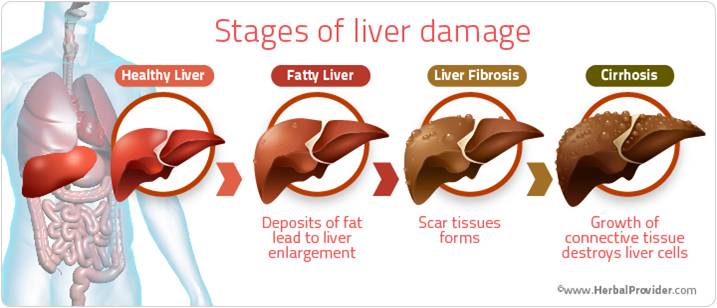
NAFLD can lead to inflammation of the liver and the formation of scar tissue, a condition called non-alcoholic steatohepatitis (NASH), which can then lead to cirrhosis of the liver. NASH usually occurs in people who are obese, have diabetes or have high blood cholesterol and triglycerides, so controlling these conditions is recommended.
Complications of liver cirrhosis
Without medical treatment, cirrhosis of the liver can lead to a range of potentially life-threatening complications including:
 insulin resistance and type 2 diabetes – a poorly functioning liver stops the body from properly using insulin, the hormone that moves sugar from the blood into the cells
insulin resistance and type 2 diabetes – a poorly functioning liver stops the body from properly using insulin, the hormone that moves sugar from the blood into the cells- osteoporosis (brittle bones) caused by changes to metabolism of calcium and vitamin D
- primary liver cancer – the most common type of cancer caused by cirrhosis is hepatocellular carcinoma
- liver failure – scar tissue can impair the functioning of normal liver tissuebleeding from blood vessels in the oesophagus or upper stomach (oesophageal varices)
- increased blood pressure in veins that take blood to the liver (portal hypertension)
- build-up of fluid within the abdominal cavity (ascites)
- infection of the fluid found within the abdominal cavity (spontaneous bacterial peritonitis)
- damage to the brain and nervous system caused by toxins that the liver has failed to remove (hepatic encephalopathy).
Treatment of liver cirrhosis
Cirrhosis of the liver is incurable but, in some cases, treatment can help to reduce the likelihood that the condition will become worse. Options include:
- treating the underlying cause of liver damage
- making dietary and lifestyle changes – a nutritious low-fat diet, high-protein diet and exercise can help people to avoid malnutrition
- avoiding alcohol – alcohol damages the liver and harms remaining healthy tissue
- Taking certain medication – such as beta-blockers to reduce blood pressure and lower the risk of bleeding, diuretics to remove excess fluid
- avoiding certain medication that can make the symptoms worse – such as non-steroidal anti-inflammatory drugs (NSAIDs), opiates or sedatives
- having regular medical check-ups – including scans to check for liver cancer
- having regular endoscopic procedures to check whether there are varicose veins within the oesophagus or stomach
- having a liver transplant – an option that may be considered in severe cases.
by Me | Oct 13, 2018 | Fatty Liver, Weight Loss Surgery Research
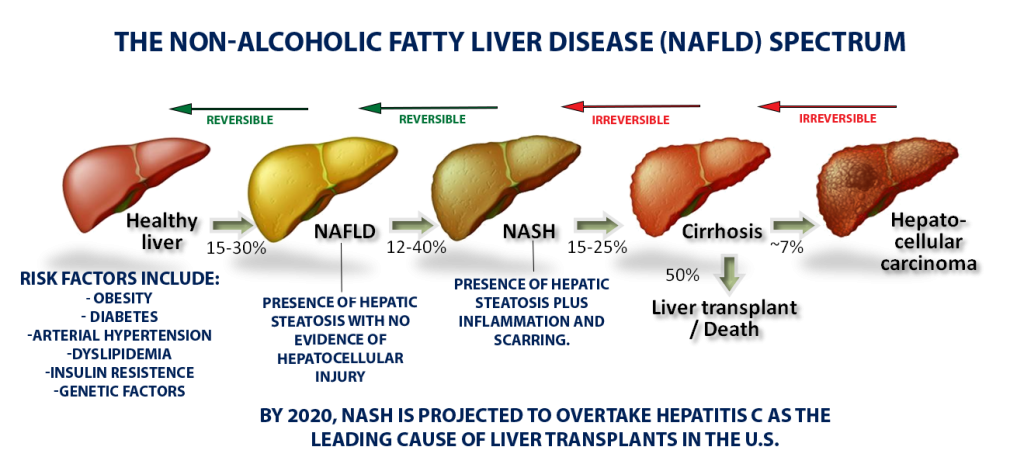
For most of us, the acronym NASH won’t ring many bells. But NASH, or NonAlcoholic SteatoHepatitis, marked by the accumulation of an unhealthy amount of fat and scar tissue in the liver, is quietly reaching epidemic proportions across the globe. By 2020, NASH is projected to overtake hepatitis C as the leading cause of liver transplants, largely because of an alarming rise in obesity and type-2 diabetes – both key risk factors for NASH.
Despite NASH’s prevalence, its obscurity isn’t all that surprising as it doesn’t cause obvious symptoms in most people, there’s no simple test to detect it, and no drugs have been approved to treat it.
Unlike high blood pressure or diabetes, which doctors can detect with cheap and easy tests during a routine check-up, NASH is difficult to diagnose. Most people with scarring on their liver don’t display symptoms, and right now there’s no straightforward biomarker that a routine blood panel would pick up. The only reliable measure of fibrosis is a liver biopsy. Also, the disease progresses slowly—over years or even decades—and researchers have yet to figure out when someone with a fatty liver is at risk for developing the inflammation and fibrosis that define NASH.
The subtle, slow-moving process begins with the build-up of fat in the liver, a condition called nonalcoholic fatty liver disease, or NAFLD, because it is not driven by alcohol consumption. For many people, a fatty liver will never become a real problem – If you have isolated fat, you may live and die with your fatty liver and never know it. But a portion of the population will go on to develop NASH’s telltale inflammation and scarring.
Anywhere from 5% to 20% of people with NASH will go on to develop cirrhosis, where scarring has stiffened the liver so much that it can no longer function properly. From there, the outcomes can be grim: liver failure, liver transplant, or liver cancer.
Right now, doctors can only recommend lifestyle changes—better diet, more exercise, less alcohol—to stop or reverse damage to the liver, which has an amazing ability to regenerate healthy cells. However, studies have shown time and again that people are unable to stick to a healthier regime, which is one reason why Bariatric Surgery (which in many ways “enforces” lifestyle changes) is considered a a viable treatment option.