by Me | Nov 30, 2018 | Diabetes, Post-Surgery

10 weeks since my surgery and time for some Statistics
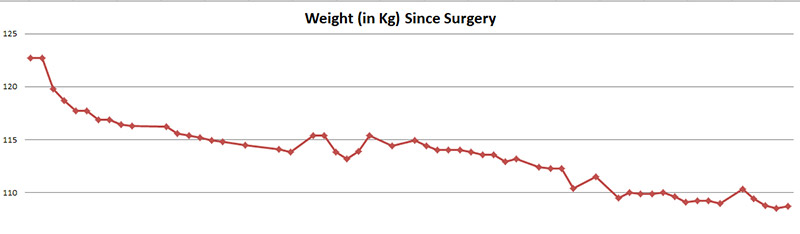
My weight continues to drop off… it has been a little erratic… losing a little each day for a week or so… putting on a kilo … and then having it drop off again.. but the overall trend is consistently down, and in the 10 weeks since surgery, I have lost a total of 14KG… and little under 1.5Kg per week is pretty good right ?:)
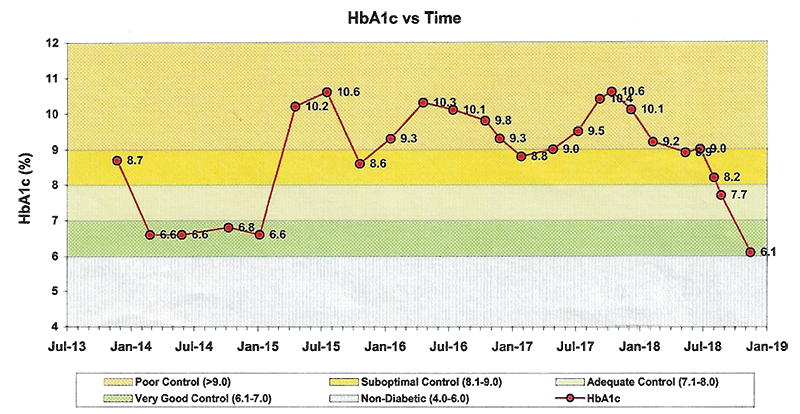
More remarkably, I am still completely medication free for my diabetes… my HbA1c Blood results have plummeted since surgery… and I am currently just a smidgeon above the “Non-Diabetic” range.
HbA1c
HbA1c is a blood test that is used to help diagnose and monitor people with diabetes. It is also sometimes called a haemoglobin A1c, glycated haemoglobin or glycosylated haemoglobin. It shows the average level blood sugar levels over the past 2 to 3 months.
The graph below shows my HbA1c stats for the last 5 years or so – since I was diagnosed with Diabetes. Soon after I was first diagnosed, I was able to control it pretty well with diet and exercise, but in 2015 it shot up and I started medication. Over the subsequent years, despite increased medication it was never really well controlled… Since late 2017 it has gradually improved, but this was primarily as a result of increase medication (mainly mutliple daily insulin injections). However, since my Gastric Bypass operation (just 10 weeks ago).. I have been complelety off all diabetes medication… and my blood sugar is almost back to “non-diabetic” levels.
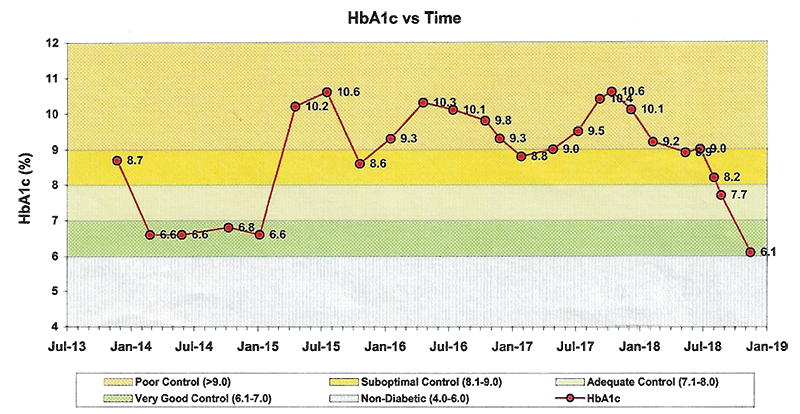
This was not entirely unexpected (and was the primary aim for the operation)… However the results have been much more dramatic than I had expected. Loss of weight in itself, is one of the most effective ways to reduce blood sugar… and I had already lost about 10Kg prior to the operation, and had seen a reduction in my medication… However weight loss is obviously a gradual thing , and the “overnight” impact on my blood sugar was a bit of a surprise… and seems to have been been as a direct result of the physiological impact of the Bariatric surgery.
Weigth Loss
The graph below shows (almost) daily weight data since my surgery10 weeks ago :
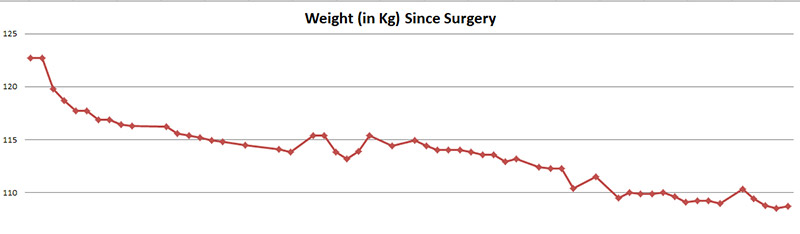
Unsurprisingly, the rate of weight loss is highest in the first week or two, but since then (apart from a few “hiccups”) has been fairly steady at about 1.5kg per week. In th4 last 10 weeks I have lost 14Kg :). The “trend” seems to be that iI lose a small, but steady daily amount (around 300g) for 7-10 days… then I put a Kg or two back on overnight, it rollercoasters for a few days… and then I start the gradual weight loss trend again. Not sure if this is related to hyydration… or diet.. or whether it is just a natural pattern.
I have not been down to this weight for about 10 years and I am “swimming” in my current wardrobe, but I am holding off getting any many new clothes until I lose a bit more 🙂
My next “major” goal is 100Kg… I will probably reward myself with some new clothes…and I have told myself that when I reach that I will start back at a gym and start to do more regular (and more “serious”) excercise.

by Me | Nov 8, 2018 | Food & Diet, Post-Surgery
The title of this post “What’s Brown and Sticky” is unfortunately the lead into one of the few jokes I seem to remember with any consistency…. It is my favourite “Dad” joke… and the answer is of course …. A Stick !!!
It is curious, that even though we don’t usually like to talk about bodily functions (in “polite” conversation)… we do seem to have a fascination with Poo and Fart jokes… and they are not just for children. Even if you’re a full-grown adult, you are still going to end up laughing your ass off. This post is primarily about Poop and Farts – in relation to Gastric Bypass Surgery, which is not quite as hilarious (but see the end of this post for some more Poop jokes).
 Apparently, after gastric bypass surgery, many people experience some degree of diarrhea and smelly gas (malodorous flatulence). This is typically common during the first few months as the body adjusts and heals.
Apparently, after gastric bypass surgery, many people experience some degree of diarrhea and smelly gas (malodorous flatulence). This is typically common during the first few months as the body adjusts and heals.
Since my Surgery (7 weeks ago), I have been Pooing much less – which is hardly surprising since I am actually eating less than half what I once would have. I have experienced a little Diarrhea (but not as much as I had anticipated), but my stools are certainly softer than pre-surgery… are consistently a light brown (almost beige) in colour… and my gas is more often than not smellier than previously.
I have collated together below a range of information on some of the most common post-surgery effects on digestion :
Digestion After Surgery
Gastric bypass surgery helps you lose weight by altering the anatomy of your digestive system. Your stomach is smaller after the procedure and food passes more
Long-Term Dietary Considerations
quickly through your digestive system. As a result, your body absorbs fewer nutrients and your shortened bowel produces more gas and odors than before surgery.
Diarrhea and flatulence usually improve as your body adjusts after gastric bypass surgery. After the early postoperative period, you will begin to eat small amounts of high-protein, low-carbohydrate, low-fat foods that give you the nutrients you need while losing weight. However, certain foods — such as meat, beans, wheat, dairy products and vegetables — may cause flatulence and diarrhea long after your body has healed.
Dumping Syndrome
Dumping syndrome frequently occurs in gastric bypass patients when they eat foods containing a large amount of sugar. The bowel responds to the high concentration of sugar by moving extra fluid into the digestive system. As a result, diarrhea may occur within 30 to 60 minutes. Excess gas is also produced as bacteria feed on the sugar. Hormones are released during an occurrence of dumping syndrome, commonly resulting in dizziness, flushing, a drop in blood pressure and an increase in heart rate. Symptoms may range from mild to severe and generally last 1 to 2 hours.
Eating Habits
Certain eating habits can increase intestinal gas. Many surgeons advise patients to avoid activities such as drinking carbonated beverages, chewing gum or using a straw to prevent the introduction of excess air into the digestive system. Eating slowly and chewing your food thoroughly can improve digestion and may reduce excess intestinal gas.
Drinking liquids during meals can push foods through the digestive system too quickly. People who have undergone gastric bypass surgery are usually advised to stop all fluids before beginning to eat and to wait for roughly 30 minutes afterward before drinking again.
More Poop Jokes
And to finish off… here are a few more Poop jokes to put a “smile” on your face :
- Did you know that diarrhea is hereditary?
It runs in your genes.
 Have you seen the movie Diarrhea?
Have you seen the movie Diarrhea?
It leaked so they had to release it early.- Did you hear about the constipated accountant?
He couldn’t budget.
- Did you hear about the constipated mathematician?
He worked it out with a pencil.
- What’s brown and sounds like a bell?
Dung.
- What did one fly say to the other?
Is this stool taken?
- Do you want to hear a poop joke?
Never mind it’s too corny.
- What’s the true definition of bravery?
Chancing a fart when you know you have diarrhea.
- Did you know that when you say the word “poop”, your mouth does the same motion as your bum hole?
The same is true for the phrase, “explosive diarrhea”.
- Poop jokes aren’t my favorite jokes.
But they’re a solid #2.

by Me | Nov 2, 2018 | Food & Diet, Post-Surgery
 6 weeks since my surgery and I am still on track
6 weeks since my surgery and I am still on track
My weight has been on a bit of a roller coaster over the last couple of weeks… going up and down a bit… I have more or less started eating “real food” so some weight gain is apparently not unusual… but overall there is still a good downward trend… and today I reached a bit of a weight milestone – under 110 Kg. I have not weighed this little for more that 5 years 🙂

My next “psychological” weight barrier is 100 KG… which I have not weighed for more than 12 years… and my target for this is Month 3…
I have been taking weekly photos, which I eventually intend collating into a timelapse…I have not noticed any dramatic changes in my body shape… although shirts are starting to feel a bit baggy…. and I will soon need to get some new undies, because my old ones are sometimes falling down when I walk 🙂
I certainly have more energy, and am building up my exercise. I currently aim for at least 6000 steps (about 5 km) each day.
I am sleeping really well.. although have been waking up earlier and earlier (usually up by 0530 these days).
 Although I am probably eating 1/3rd of what I used to, I am still not feeling hungry at all, and have to remind myself to eat. As expected I can only manage small quantities of food at a time… A couple of poached eggs and 1 piece of toast or a muffin is too much for me to eat in one go…
Although I am probably eating 1/3rd of what I used to, I am still not feeling hungry at all, and have to remind myself to eat. As expected I can only manage small quantities of food at a time… A couple of poached eggs and 1 piece of toast or a muffin is too much for me to eat in one go…
I have also started to make up batches of fresh seasonal fruit salad (watermelon, rockmelon, pineapple, banana, strawberries, passionfruit, grapes at the moment)… and am enjoying eating this a couple of times a day as snacks.
by Me | Oct 22, 2018 | Fatty Liver
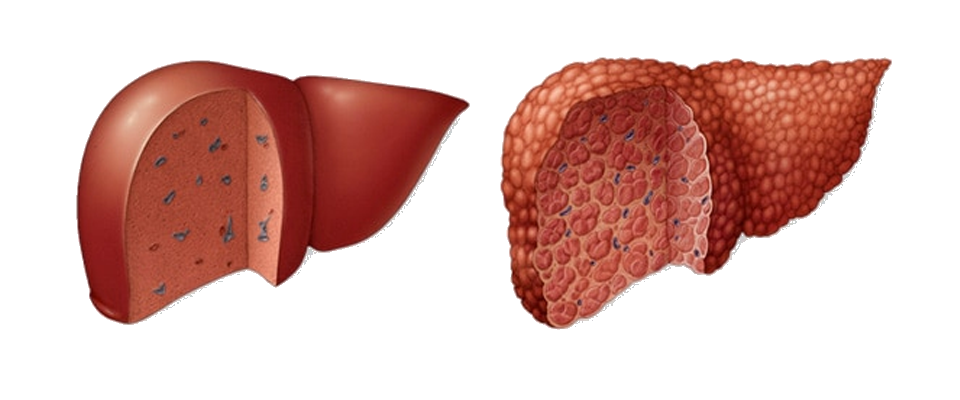
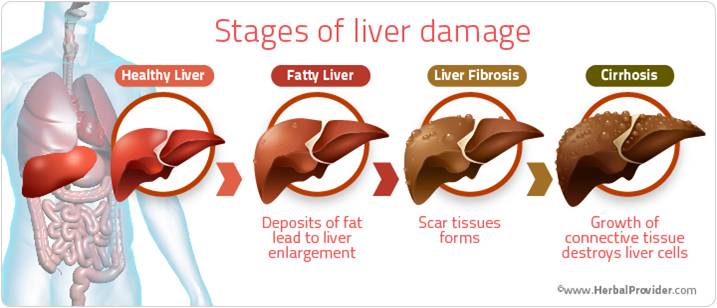
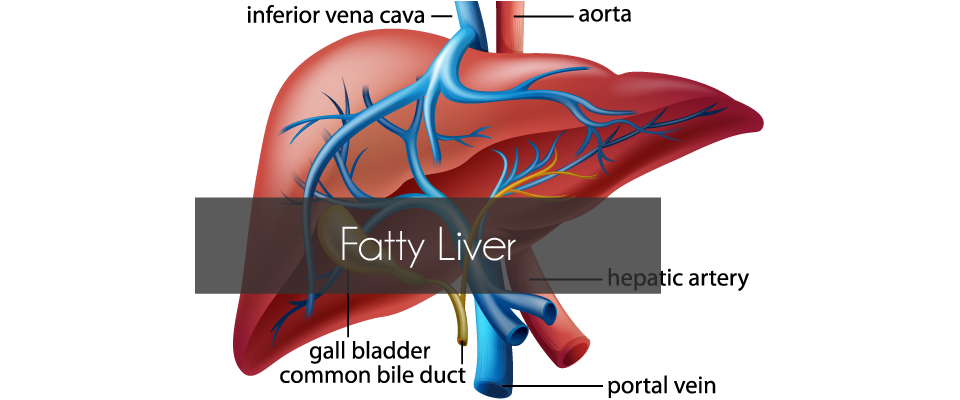
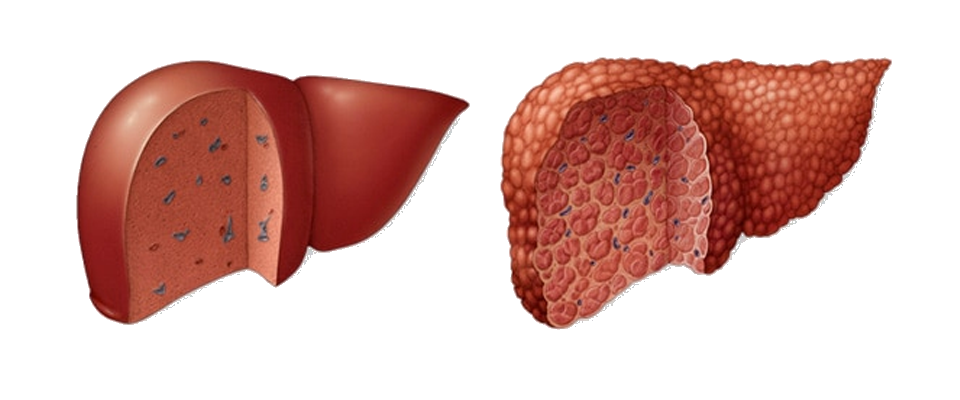
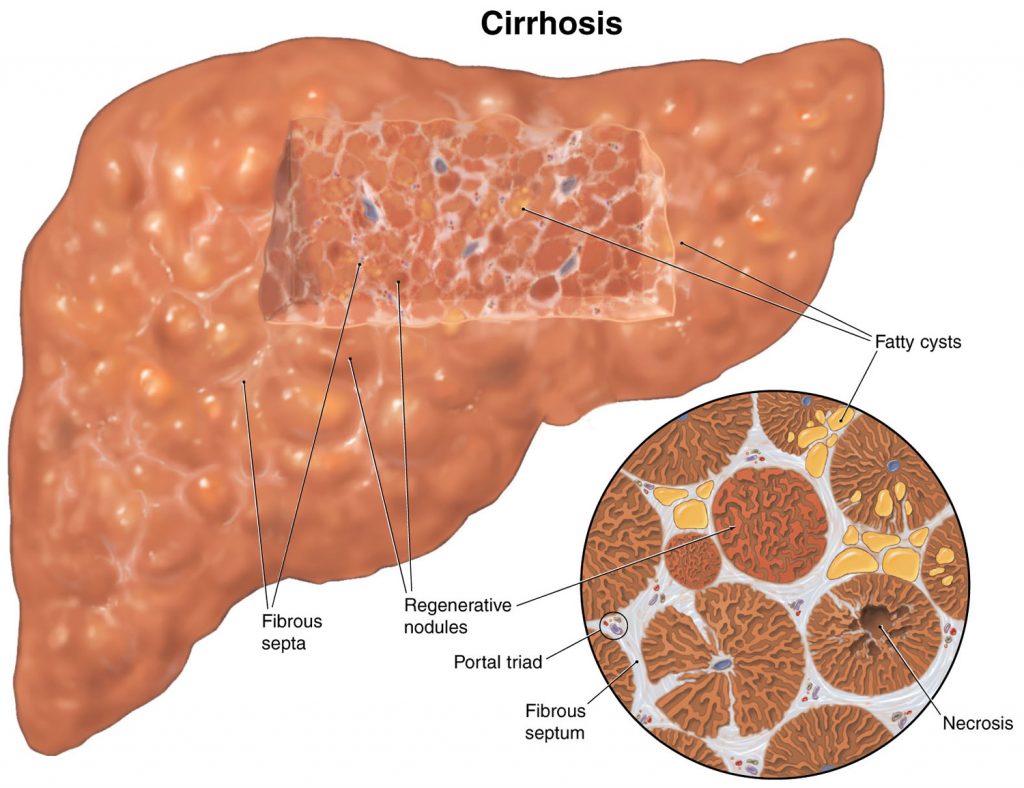
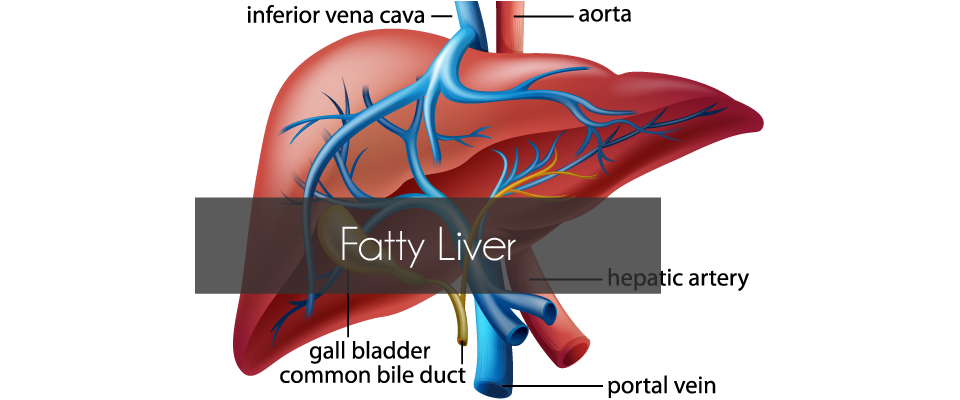
I have been aware that I have had a fatty liver for some time…. Although my liver function is fine, ultrasounds over the last few years have shown that it is enlarged (which is not unusual with obesity) and a Fibroscan undertaken last year indicated that it was probably scarred (and potentially cirrhotic), but it was not until a liver biopsy was taken during my gastric bypass surgery, that Cirrhosis of the liver has been confirmed.
Cirrhosis is scarring of the liver caused by long-term liver damage. … Cirrhosis can eventually lead to liver failure, where your liver stops working, which can be fatal. But it usually takes years for the condition to reach this stage and treatment can help slow its progression.
Cirrhosis is a type of liver damage where healthy cells are replaced by scar tissue. The liver is unable to perform its vital functions of metabolism, production of proteins, including blood clotting factors, and filtering of drugs and toxins. A common misconception is that liver cirrhosis is caused by drinking excessive amounts of alcohol, but there are a number of other ways that the liver can be damaged and lead to cirrhosis.
Liver cirrhosis and fatty liver
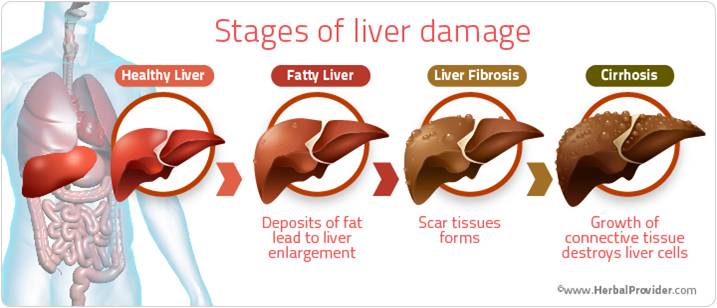
Non-alcoholic fatty liver disease (NAFLD) is a condition where fat accumulates in the liver. It now affects about 20 per cent of Australians. It is becoming more common in children who are overweight or obese. Fatty liver does not usually cause pain or nausea. NAFLD is associated with conditions such as:
- obesity – 20 per cent of people with obesity have fatty liver disease
- high blood cholesterol and triglycerides
- type 2 diabetes.
NAFLD can lead to inflammation of the liver and the formation of scar tissue, a condition called non-alcoholic steatohepatitis (NASH), which can then lead to cirrhosis of the liver. NASH usually occurs in people who are obese, have diabetes or have high blood cholesterol and triglycerides, so controlling these conditions is recommended.
Complications of liver cirrhosis
Without medical treatment, cirrhosis of the liver can lead to a range of potentially life-threatening complications including:
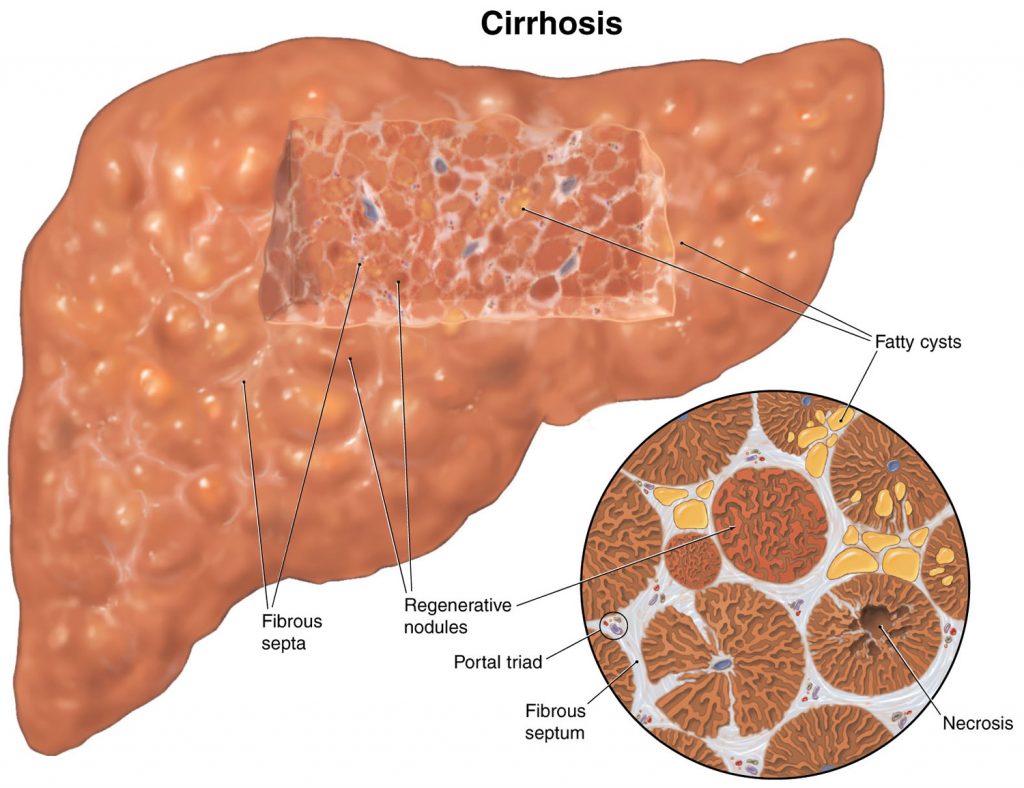 insulin resistance and type 2 diabetes – a poorly functioning liver stops the body from properly using insulin, the hormone that moves sugar from the blood into the cells
insulin resistance and type 2 diabetes – a poorly functioning liver stops the body from properly using insulin, the hormone that moves sugar from the blood into the cells- osteoporosis (brittle bones) caused by changes to metabolism of calcium and vitamin D
- primary liver cancer – the most common type of cancer caused by cirrhosis is hepatocellular carcinoma
- liver failure – scar tissue can impair the functioning of normal liver tissuebleeding from blood vessels in the oesophagus or upper stomach (oesophageal varices)
- increased blood pressure in veins that take blood to the liver (portal hypertension)
- build-up of fluid within the abdominal cavity (ascites)
- infection of the fluid found within the abdominal cavity (spontaneous bacterial peritonitis)
- damage to the brain and nervous system caused by toxins that the liver has failed to remove (hepatic encephalopathy).
Treatment of liver cirrhosis
Cirrhosis of the liver is incurable but, in some cases, treatment can help to reduce the likelihood that the condition will become worse. Options include:
- treating the underlying cause of liver damage
- making dietary and lifestyle changes – a nutritious low-fat diet, high-protein diet and exercise can help people to avoid malnutrition
- avoiding alcohol – alcohol damages the liver and harms remaining healthy tissue
- Taking certain medication – such as beta-blockers to reduce blood pressure and lower the risk of bleeding, diuretics to remove excess fluid
- avoiding certain medication that can make the symptoms worse – such as non-steroidal anti-inflammatory drugs (NSAIDs), opiates or sedatives
- having regular medical check-ups – including scans to check for liver cancer
- having regular endoscopic procedures to check whether there are varicose veins within the oesophagus or stomach
- having a liver transplant – an option that may be considered in severe cases.

by Me | Oct 21, 2018 | Food & Diet, Post-Surgery
OK… I’ve survived 2 weeks of liquids and 2 weeks of mush puree… for the next 2 weeks I graduate to “soft food”
Here are the “key points of my diet for the next 2 weeks :
- Separate Liquids from Solids – wait 10 minutes before eating and 30 minutes after eating before having something to drink
- Eat Mindfully – take it slowly (30 seconds between mouthfulls) and Chew Chew Chew…Stop eating as soon as I start feeling full
- Focus on Proteins and Fluids (for faster recovery and muscle mass maintenance) – and eat protein First.
- Daily Multivitamin / Calcium Supplements (I will probably be taking these for the rest of my life)
- Avoid High Kilojoule fluids (these will slow down weight loss)
- Aim for 3 small meals a day – with 1-2 healthy snacks if physically hungry
Here are some of the things I could/should be eating for different meals :
Breakfast
 High Fibre cereal and with low fat milk
High Fibre cereal and with low fat milk- Bircher Muesli
- Oats/Porridge
- Scrambled/Poached egg
- Soft Fruit
Lunch
- Omelette/Frittata
 Fresh Salad with lean protein
Fresh Salad with lean protein- Mini wrap with lean protein and salad
Dinner
- Mince based meals with softly cooked veggies
- Slow cooked casseroles
- Steamed/poached fish
- (minimise pasta/rice/noodles/potato)
Healthy Snacks
 Low fat yoghurt
Low fat yoghurt- 1 piece of soft fruit (banana, melon, berries)
- Low fat cheese (cottage cheese or Babybel Light)

by Me | Oct 20, 2018 | Food & Diet, Post-Surgery
1 month know since my surgery and I am still feeling awesome !!!
I have still lost 9Kg since surgery a month ago (I actually put on some weight a couple of days this week – which is apparently not unusual) and am still feeling great…
I saw the dietician again yesterday – and had my 1st post-surgery checkup with the surgeon…
I have a new food plan for the next 2 weeks (week 5 & 6), which I will post about separately… and I need to drink more water (I’ve been a bit slack on hydration). but I am mostly (apart from the odd sausage roll and pizza) on track food-wise.
My liver biopsy (taken during surgery) has come back positive for Cirrhosis – which is a shame, but not unexpected. I will create a separate post/page about Liver Cirrhosis and it’s implications… but I am VERY glad that the surgeon decided to proceed with the Gastric Bypass – as this is the best “treatment” for my liver issues.
I am still medication free for Diabetes (and have been for a month), and my blood sugar is behaving very nicely 🙂
by Me | Oct 13, 2018 | Fatty Liver, Weight Loss Surgery Research
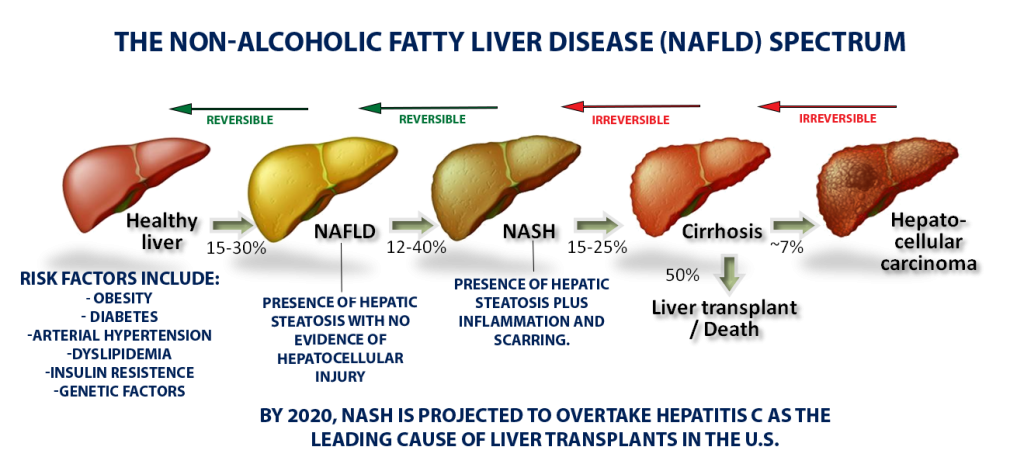
For most of us, the acronym NASH won’t ring many bells. But NASH, or NonAlcoholic SteatoHepatitis, marked by the accumulation of an unhealthy amount of fat and scar tissue in the liver, is quietly reaching epidemic proportions across the globe. By 2020, NASH is projected to overtake hepatitis C as the leading cause of liver transplants, largely because of an alarming rise in obesity and type-2 diabetes – both key risk factors for NASH.
Despite NASH’s prevalence, its obscurity isn’t all that surprising as it doesn’t cause obvious symptoms in most people, there’s no simple test to detect it, and no drugs have been approved to treat it.
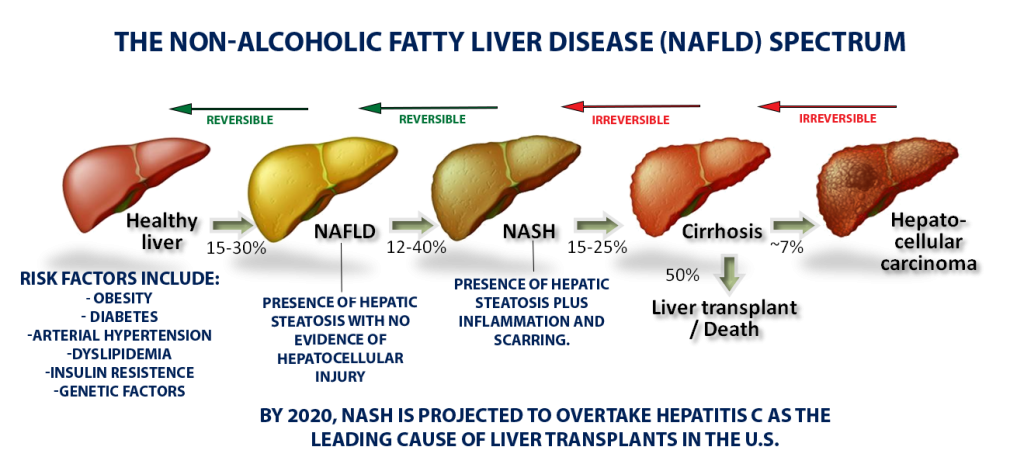
Unlike high blood pressure or diabetes, which doctors can detect with cheap and easy tests during a routine check-up, NASH is difficult to diagnose. Most people with scarring on their liver don’t display symptoms, and right now there’s no straightforward biomarker that a routine blood panel would pick up. The only reliable measure of fibrosis is a liver biopsy. Also, the disease progresses slowly—over years or even decades—and researchers have yet to figure out when someone with a fatty liver is at risk for developing the inflammation and fibrosis that define NASH.
The subtle, slow-moving process begins with the build-up of fat in the liver, a condition called nonalcoholic fatty liver disease, or NAFLD, because it is not driven by alcohol consumption. For many people, a fatty liver will never become a real problem – If you have isolated fat, you may live and die with your fatty liver and never know it. But a portion of the population will go on to develop NASH’s telltale inflammation and scarring.
Anywhere from 5% to 20% of people with NASH will go on to develop cirrhosis, where scarring has stiffened the liver so much that it can no longer function properly. From there, the outcomes can be grim: liver failure, liver transplant, or liver cancer.
Right now, doctors can only recommend lifestyle changes—better diet, more exercise, less alcohol—to stop or reverse damage to the liver, which has an amazing ability to regenerate healthy cells. However, studies have shown time and again that people are unable to stick to a healthier regime, which is one reason why Bariatric Surgery (which in many ways “enforces” lifestyle changes) is considered a a viable treatment option.

by Me | Oct 12, 2018 | Food & Diet, Post-Surgery

3 weeks know since my surgery and I am still feeling GREAT !!!
I have now lost 9Kg since surgery and am still feeling great… and continue to lose weight – but today… for the first time (probably of many) I Threw Up !!!
I was warned to expect this.. getting used to quantities and types of food I can eat is a normal part of the process… but it still came as a little bit of a surprise… I admit I am pushing the envelope a little on my diet, and today I thought I could manage a sausage roll – as long as I chewed it up well.
 I did manage three quarters of it before I started to feel full and a little uncomfortable (which is not unusual), so I stopped. However, this time, after about 5 minutes I suddenly (without any warning) felt the need to throw up.
I did manage three quarters of it before I started to feel full and a little uncomfortable (which is not unusual), so I stopped. However, this time, after about 5 minutes I suddenly (without any warning) felt the need to throw up.
It wasn’t much … just a couple of mouthfulls… but interestingly (to me anyway), it wasn’t the sausage roll that I threw up, it was a clear slimy “liquid”…. no sausage roll (chewed or otherwise) in sight.
OK… I know I should still really be on “mush” (I have another week officially) but in the last few days I have been eating a few “other” things (some chips, some BBQ shapes), but consciously chewing them very well before swallowing.
I know once I start “eating real food”, that throwing up is a normal part of the process in coming to terms with the types and quantities of food that I can eat… and I have been told that the “types” of food can be a more significant factor that the quantity. In this case, I didn’t eat very much, but I am guessing my new stomach is not used to high carb/fatty foods.
I promise to eat better (at least until my next appointment next week with the dietician/surgeon) 🙂
 p.s. although I was tempted… I didn’t go back later and finish off he sausage roll 🙂
p.s. although I was tempted… I didn’t go back later and finish off he sausage roll 🙂

by Me | Oct 7, 2018 | Diabetes, Food & Diet, Weight Loss Surgery Research
One of the main reasons I went ahead with Weight Loss Surgery was to manage/control my Diabetes II. After several years of trying diet and exercise, the medications I needed to keep my blood sugar under control were increasing. I am now very happy to say that since my surgery (just over 2 weeks ago), I have stopped all diabetes medication and my blood sugar remains completely normal.
I didn’t believe I was able to manage my Diabetes by diet alone… but recent research suggest that diet drinks and artificial sweeteners (which I used to have regularly) has a link to increased risk for Diabetes II.
 I am satisfied that there was no direct link with my Blood Sugar readings and consumption of diet soda (I used to have 2 and up to 6 cans of Pepsi Max a day)… These drinks are “sugar free” and I could see that my blood sugar was unaffected 1-3 hrs after consumption (whereas I could see spikes in blood sugar after eating carbs/sugary food)… However research by the Adelaide Medical School has found that high intake of low-calorie sweeteners (like those found in diet drinks) over just two weeks was enough to significantly alter the make-up of bacteria in the gut… which in turn effects the way the body absorbs and regulates blood sugar – increasing the risk of developing diabetes over time.
I am satisfied that there was no direct link with my Blood Sugar readings and consumption of diet soda (I used to have 2 and up to 6 cans of Pepsi Max a day)… These drinks are “sugar free” and I could see that my blood sugar was unaffected 1-3 hrs after consumption (whereas I could see spikes in blood sugar after eating carbs/sugary food)… However research by the Adelaide Medical School has found that high intake of low-calorie sweeteners (like those found in diet drinks) over just two weeks was enough to significantly alter the make-up of bacteria in the gut… which in turn effects the way the body absorbs and regulates blood sugar – increasing the risk of developing diabetes over time.
The researchers recruited 27 healthy subjects who were given a quantity of two different non-caloric artificial sweeteners (sucralose and acesulfame-K) equivalent to drinking 1.5L of diet beverage per day, or an inactive placebo.
The study determined that just 2 weeks of NAS supplements was enough to enhance glucose absorption and increase the magnitude of the response of blood glucose as a result. The authors conclude that “This study supports the concept that artificial sweeteners could reduce the body’s control of blood sugar levels and highlights the potential for exaggerated post-meal glucose levels in high habitual NAS users, which could predispose them to developing type 2 diabetes”.
The same Researchers are now setting out to prove for the first time if these sweeteners are actually impairing blood glucose control in type 2 diabetes sufferers rather than improving it, as has always been believed.

by Me | Oct 4, 2018 | Diabetes, Post-Surgery
Well no… Not Really… I am not actually cured (I still have susceptibility to Diabetes II), but at the moment my blood sugar is being controlled without the need for medication. Medically speaking, there is no cure for diabetes but it can go into “remission.” Diabetes in remission simply means the body does not show any signs of diabetes. However, the disease is technically still there.
I was diagnosed with Diabetes II in several years ago, and since then have been battling to control my blood sugar – initially with diet/exercise, but for the last couple of years I have required medication and Insulin injections.

The long term effects of Diabetes are NASTY…(increased risk of heart attack and stroke, and problems with the kidneys, eyes, feet and nerves)…. and controlling my Diabetes is one of the main reasons I decided to go ahead with Bariatric Surgery – the weight loss was a convenient side effect 🙂
I had actually lost about 10Kg in weight prior to surgery (primarily because I lost my sense of taste) and I had already significantly cut down on medications before I even had the surgery… Bariatric Surgery is also known to reduce the dependency on medication to control Blood Sugar – partly because of the associated weight loss, but also because it seems to change the way the gut behaves (changes typically occur even before weight loss could be considered a contributory factor)
I have not had ANY Diabetes medication since the evening of my surgery and my blood sugar has been a very stable 6ish… although I need to keep monitoring regularly because once I start on food again (even mush) I am anticipating that this may change.









 High Fibre cereal and with low fat milk
High Fibre cereal and with low fat milk Fresh Salad with lean protein
Fresh Salad with lean protein Low fat yoghurt
Low fat yoghurt



 I did manage three quarters of it before I started to feel full and a little uncomfortable (which is not unusual), so I stopped. However, this time, after about 5 minutes I suddenly (without any warning) felt the need to throw up.
I did manage three quarters of it before I started to feel full and a little uncomfortable (which is not unusual), so I stopped. However, this time, after about 5 minutes I suddenly (without any warning) felt the need to throw up. p.s. although I was tempted… I didn’t go back later and finish off he sausage roll 🙂
p.s. although I was tempted… I didn’t go back later and finish off he sausage roll 🙂
 I am satisfied that there was no direct link with my Blood Sugar readings and consumption of diet soda (I used to have 2 and up to 6 cans of Pepsi Max a day)… These drinks are “sugar free” and I could see that my blood sugar was unaffected 1-3 hrs after consumption (whereas I could see spikes in blood sugar after eating carbs/sugary food)… However research by the Adelaide Medical School has found that high intake of low-calorie sweeteners (like those found in diet drinks) over just two weeks was enough to significantly alter the make-up of bacteria in the gut… which in turn effects the way the body absorbs and regulates blood sugar – increasing the risk of developing diabetes over time.
I am satisfied that there was no direct link with my Blood Sugar readings and consumption of diet soda (I used to have 2 and up to 6 cans of Pepsi Max a day)… These drinks are “sugar free” and I could see that my blood sugar was unaffected 1-3 hrs after consumption (whereas I could see spikes in blood sugar after eating carbs/sugary food)… However research by the Adelaide Medical School has found that high intake of low-calorie sweeteners (like those found in diet drinks) over just two weeks was enough to significantly alter the make-up of bacteria in the gut… which in turn effects the way the body absorbs and regulates blood sugar – increasing the risk of developing diabetes over time.
